India’s healthcare infrastructure is on the brink of collapse and hospitalizations, and deaths are shattering records every other day. Even if we achieve a peak, covid will continue to flare up in waves as soon as we have our guard down. As far as defeating coronavirus goes, experts have unanimously agreed that vaccination is our only weapon. While vaccine supply is a bigger problem to tackle in the short term, let’s explore another problem that has the potential to derail our plans for complete immunization.
The debate over which vaccine is the best has had a major impact on geopolitics and consequently our response to the pandemic. The efficacy rate has been at the forefront of this debate. In this article, we will discuss why getting any approved vaccine may be sensible and why it’s pointless to compare efficacy rates across vaccines.
Over the past year, governments, pharma companies and institutions have created a perception that efficacy rate is the most important parameter for the effectiveness of a vaccine. This has had an impact on funding R&D, capacity building and public perception of vaccines in general. When politicians are swayed by this perception, it causes a more profound effect. French President Emmanuel Macaron’s critique of the Oxford jab in February caused a ripple effect in France as people lining up to take the shot deliberately missed appointments. For a mass vaccination to be effective, we need to achieve herd immunity and this would require at least 70% of the entire population to be vaccinated. If there is a seed of doubt, that certain vaccines are ineffective or cause harm, this escalates into a chain reaction, leaving a significant population not wanting to vaccinate and thus curtail our ability to reach the 70% mark.
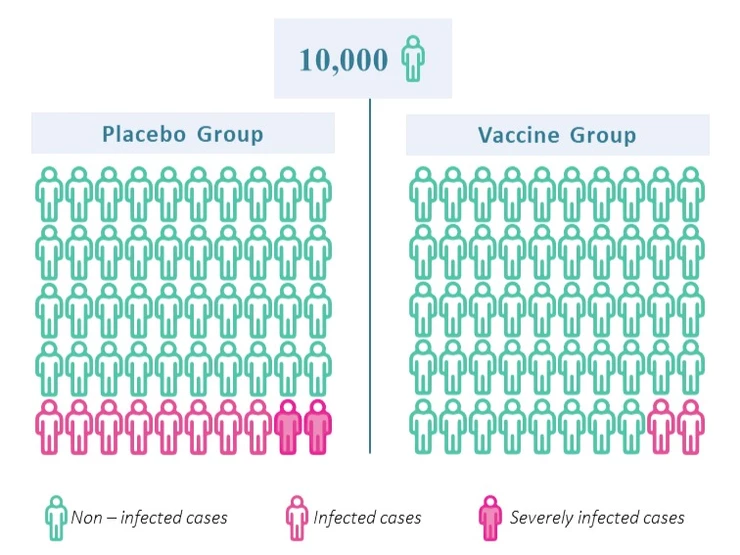
But first, let us first understand what efficacy even means. A vaccine’s efficacy rate is calculated in large clinical trials wherein the vaccine is tested on thousands of people. The volunteers are divided into two groups – Group A, those who get the vaccine, and Group B, those who get a placebo. The groups are then monitored over a period of time. Let us say that there were 10,000 people in the trial, split into groups of 5,000 each. If there were 10 people infected in Group A (Vaccine Group) and 50 people infected in Group B (Placebo Group), the efficacy rate will be 80% (1-10/50). This does not mean that out of 100 people vaccinated 20 will get sick. This number indicates that every vaccinated individual is 80% less likely to get sick.
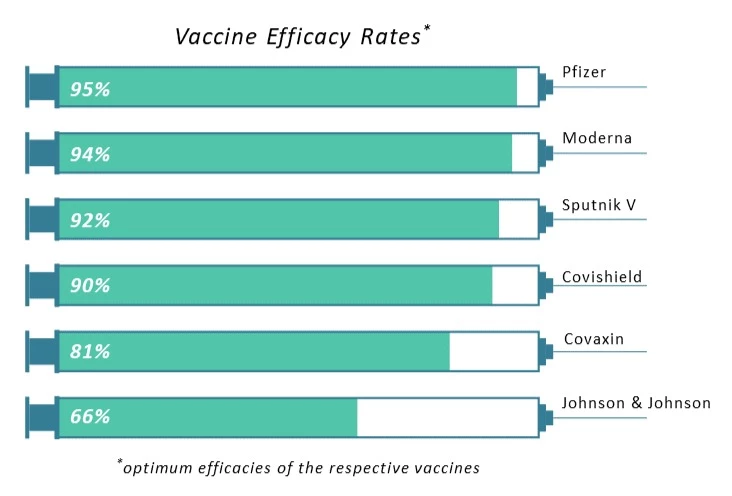
However, this efficacy rate cannot be compared across vaccines due to variation in the factors affecting their respective trials. Not only did companies like Pfizer and Moderna conduct their trials in the early stages of the pandemic, but they also restricted themselves to certain geographical areas. Therefore, only a limited number of people had the chance to get infected, thus giving a much higher efficacy rate (~95%). On the other hand, companies like J&J conducted their trials on a larger geographical scale and at a time when the infections were at their peak. The efficacy rate, in this case, was relatively low (~66%). Therefore, it’s tough to conclude whether any vaccine is better than the other just by looking at its efficacy rates. It’d be interesting to see if the efficacy rates of these vaccines will be the same if the trials were conducted today in India.
This difficulty of comparing efficacy rates is not even the most important reason we should stop obsessing over these numbers. Irrespective of the efficacy rates, all the vaccines developed till date (including Covishield and Covaxin) have been successful in lowering the hospitalization rate significantly and preventing deaths. This has been clearly evident from clinical trials, wherein even if people contracted covid after vaccination, very small number of people developed serious complications. Additionally, as per this US study, the Pfizer and Moderna vaccines reduced hospitalizations by 94% among older adults, the most vulnerable people. And this study was based on public use data and not clinical trial data.
Efficacy rates do matter for vaccines, but it may not be the most important metric to judge the covid vaccine with. It’s important to realize that the ultimate aim of vaccine is not to eliminate the virus completely, but to cripple its ability to cause serious complications and make it harmless. So let us stop our romanticization with efficacy rates and get vaccinated with any approved vaccine out there.